If you’re under 50, colorectal cancer probably isn’t on your radar. It should be.
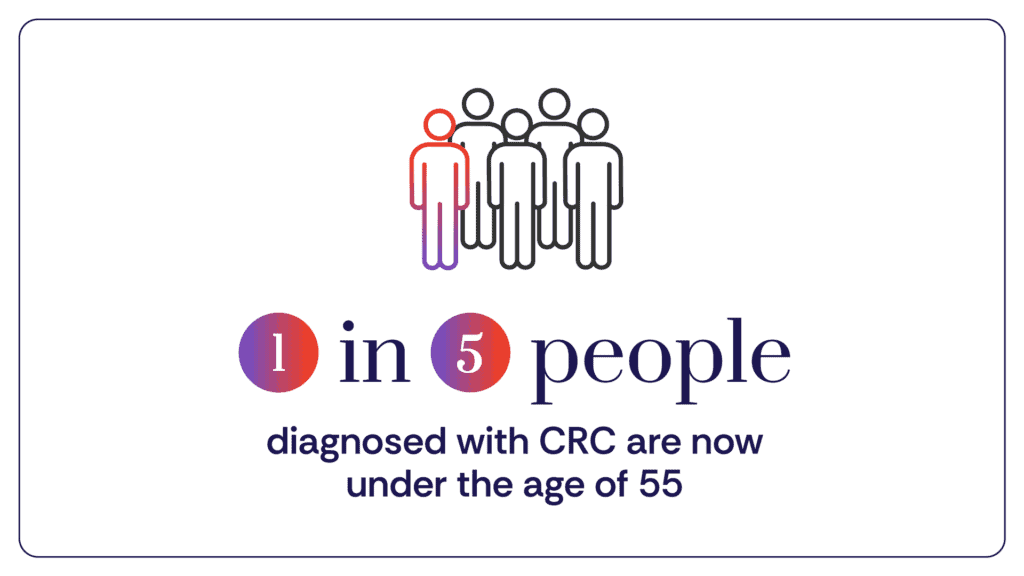
Once considered a disease of older age, colorectal cancer is rising at an alarming rate in younger adults. Today, 1 in 5 diagnoses occurs in someone under the age of 55 — and it has become a leading cause of cancer-related death in young people.
Understanding your risk factors – and acting early – could make all the difference.
The Facts
In the United States, colon cancer and rectal cancer – collectively known as colorectal cancer (CRC) – is the third most commonly diagnosed cancer and the third leading cause of cancer-related death in both men and women. The American Cancer Society (ACS) estimates that in 2026 alone, approximately 108,860 new cases of CRC will be diagnosed in the US, with about 55,230 deaths.
The lifetime risk is sobering: about 1 in 25 men and 1 in 26 women will develop colorectal cancer.
Even more concerning, cases of CRC are on the rise in younger adults. Today, 1 in 5 people diagnosed with CRC is under age 55, and it is now the leading cause of cancer-related death among young adults. Once considered primarily a disease of older age, CRC is rising at an alarming rate in people under 50 – by nearly 3% per year – even as incidence has declined slightly in the overall population.
Experts estimate that more than half of CRC cases in the U.S. may be linked to modifiable risk factors, including diet, physical inactivity, smoking, and alcohol use. Understanding these risks – and taking proactive steps – can make a meaningful difference.
March is Colorectal Cancer Awareness Month. Here’s what you need to know.
Understanding Your Risk
A combination of factors shapes your risk of developing CRC — some within your control and others beyond it.
Risk Factors Within Your Control
Diet
A diet high in processed and red meats and low in fiber, fruits, and vegetables is associated with increased CRC risk. The World Cancer Research Fund recommends limiting red meat consumption to 12–18 ounces per week and minimizing processed meats.
Physical Inactivity and Obesity
Excess body weight and a sedentary lifestyle are linked to higher colorectal cancer rates. Regular physical activity – even 30 to 60 minutes of walking daily – can support overall colon health.
Smoking and Alcohol Use
Long-term smoking and heavy alcohol consumption increase CRC risk. Quitting smoking and moderating alcohol intake can significantly reduce your risk. Speak with your healthcare provider about support options.
Risk Factors Beyond Your Control
Age
Risk increases with age, particularly after 50, though rising rates in younger adults underscore the importance of awareness at every age.
Family History and Genetics
A family history of colorectal cancer or colon polyps increases your risk. Inherited conditions such as Lynch syndrome, familial adenomatous polyposis (FAP), and MYH-associated polyposis also significantly elevate risk. Individuals with these conditions should discuss early and more frequent screening with their physician.
Race and Ethnicity
American Indian and Alaska Native populations have the highest CRC incidence rates in the U.S., followed by African Americans.
Chronic Inflammatory Conditions
Long-standing inflammatory bowel diseases, including ulcerative colitis and Crohn’s disease, can increase CRC risk due to chronic inflammation of the colon.
Understanding your risk factors isn’t meant to create fear — it’s meant to empower you. Many risks are modifiable, and informed action can save lives.
Learn more about cancer prevention tips.

The Care Gap
Healthcare disparities also contribute to rising CRC rates. Communities with high poverty levels and limited access to healthcare experience disproportionately high mortality rates. Limited access to early screening and timely treatment can delay diagnosis and worsen outcomes.
For example, Alaska Native populations experience some of the highest CRC incidence rates, influenced by a combination of genetic factors, dietary patterns, and barriers to screening access.
Addressing these disparities requires expanding access to screening, prevention, and high-quality treatment across all communities. Progress is being made — but more work remains to ensure equitable care for everyone.
Know the Symptoms
Early symptoms of colorectal cancer can be subtle. Pay attention to:
- Changes in bowel habits (persistent diarrhea or constipation)
- Blood in the stool
- Abdominal pain or cramping
- Unexplained weight loss
- Fatigue or low iron levels
If you experience any of these symptoms, don’t ignore them. Schedule an appointment with your doctor to discuss your concerns.
Early Detection Saves Lives
Colorectal cancer is often preventable — and highly treatable when detected early.
Screening guidelines generally recommend beginning regular screening at age 45. If you have additional risk factors, you may need to start earlier. Talk with your doctor about the right screening plan for you.
Common Screening Options:
Colonoscopy
The gold standard for CRC screening. A flexible, camera-equipped scope examines the entire colon and rectum and can remove precancerous polyps during the same procedure.
Stool-Based Tests
These tests detect blood or abnormal DNA in stool samples. Some options can be completed at home.
Blood-Based Screening Tests
In 2024, the FDA approved the first blood test for colorectal cancer screening. These tests detect tumor-derived DNA fragments in the bloodstream, offering a less invasive option that may increase screening participation. While promising, they do not replace colonoscopy for all patients and should be discussed with a healthcare provider.
Advances in screening are helping detect CRC earlier—when it is most treatable.
Treatment Options: There is Hope
A colorectal cancer diagnosis can feel overwhelming — but effective treatment options are available.
Treatment depends on the stage of the cancer and its molecular characteristics:
- Early-stage disease is often treated with surgery, sometimes followed by chemotherapy or radiation, depending on tumor features.
- Advanced disease may require a combination of surgery, chemotherapy, radiation, targeted therapy, and immunotherapy.
- Immunotherapy, in particular, has transformed outcomes for certain patients by harnessing the power of the immune system to fight cancer.
Research continues to expand treatment possibilities and improve survival outcomes.
Let’s Spread the Word!
This Colorectal Cancer Awareness Month, let’s normalize conversations about gut health and screening. Ask the right questions about your risk factors and take the steps to reduce them.
Share this information with friends and family. Encourage loved ones to understand their risk, recognize symptoms, and stay up to date with screening.
Together, we can raise awareness, expand access to prevention and treatment, and move closer to a world immune to cancer.
https://acsjournals.onlinelibrary.wiley.com/doi/10.3322/caac.70043
https://www.cancer.org/cancer/types/colon-rectal-cancer/causes-risks-prevention/risk-factors.html
https://www.yalemedicine.org/news/colorectal-cancer-in-young-people
https://jamanetwork.com/journals/jama/article-abstract/2844189
https://pubmed.ncbi.nlm.nih.gov/40438851
https://pubmed.ncbi.nlm.nih.gov/33208026/ https://www.nccn.org/professionals/physician_gls/pdf/colorectal_screening.pdf
