
The CRI Timeline
Funding 70 Years of Discovery in Cancer Immunotherapy
The CRI Timeline
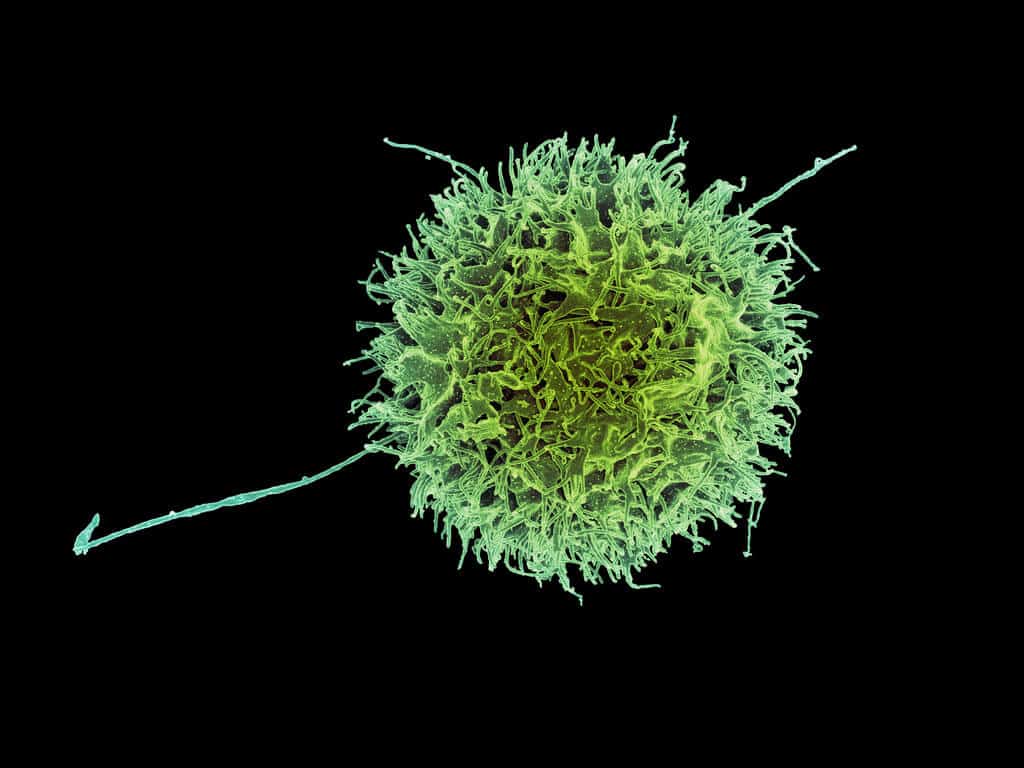
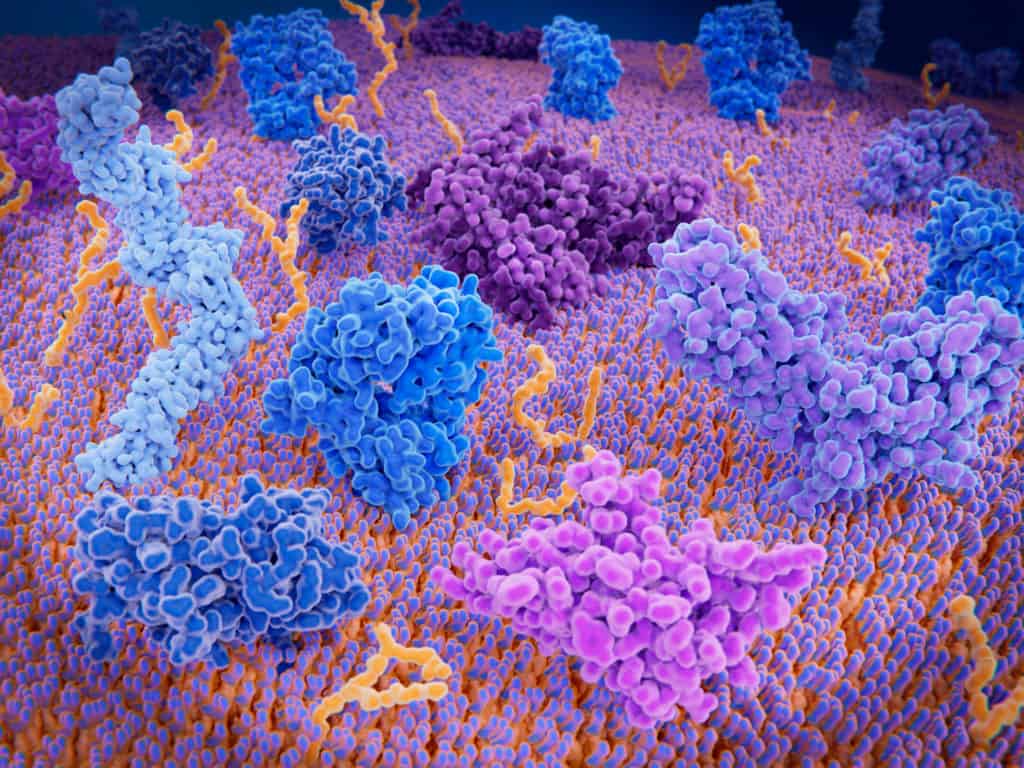
In recent decades, the number of people dying from cancer in the U.S. has declined by almost one-third – a statistic that translates into hope and relief for patients and their families. Advances in treating cancer patients with immunotherapy, improved screening, and earlier diagnosis are largely credited with this progress.
Immunotherapy is now a beacon of hope for millions of patients worldwide treated with it each year, and the scientific consensus is now irrefutable: cancer immunotherapy is a modern and innovative way to treat cancer. The journal Science named immunotherapy “Scientific Breakthrough of the Year” in 2013, and immunotherapy continues to benefit more patients each year. Up to one-third of all cancer patients are now eligible for treatment with immunotherapy and have new treatment options and more hope for living longer.
The Cancer Research Institute (CRI) established and continues to foster the field of cancer immunotherapy since its official incorporation on January 27, 1953. From the dedicated work of the thousands of scientists who have received funding from CRI since 1953, CRI has produced important discoveries that have driven progress in cancer treatment not seen since the 1940s.
Although the job is not yet complete, we invite you to learn about the institutional milestones, scientific discoveries, and people involved in making CRI the primary authority in cancer immunotherapy that it is today.
View the entire CRI timeline below.
1950s
A New Vision for Cancer Treatment is Given a Home
1953
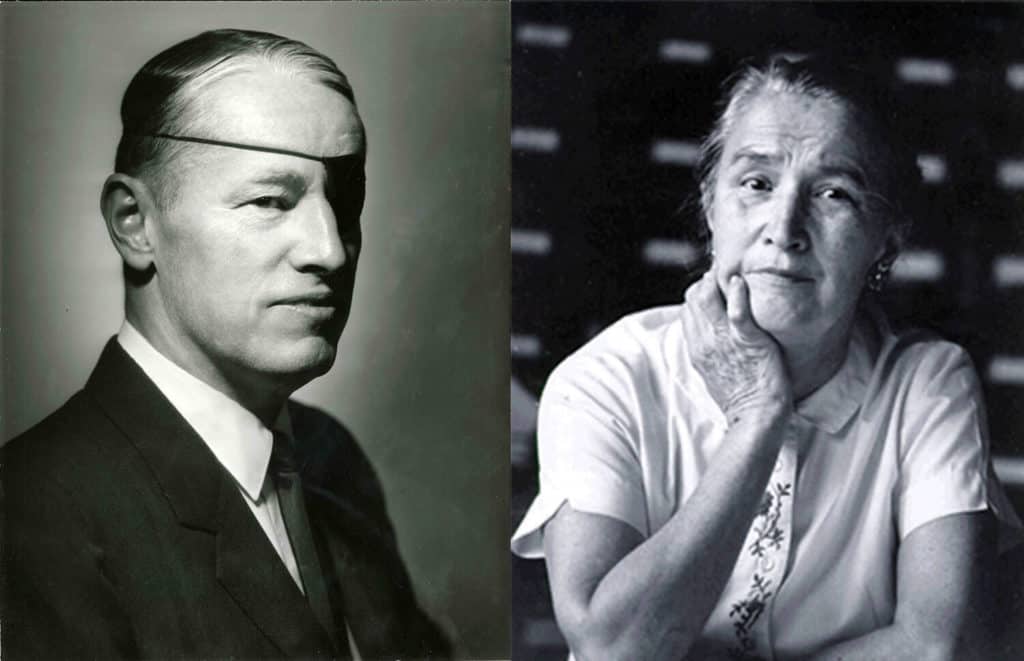
CRI Is Founded as First Nonprofit to Advance Cancer Immunotherapy Research
CRI is founded in 1953 by Helen Coley Nauts and Oliver R. Grace Sr., with a $2,000 grant from Nelson Rockefeller, whose father, John D. Rockefeller Jr., had lost a beloved friend, Elizabeth “Bessie” Dashiell, to cancer. Helen’s father, William B. Coley, MD, a renowned New York City surgeon in the late 1890s and early 1900s, had begun to experiment with a new way to treat inoperable cancers with a formulation he invented called mixed bacterial toxins, or now “Coley’s Toxin.”
Helen’s father discovered that injecting his toxin directly into tumors could result in cures for some of his patients. Helen pursued her father’s work with a passion and devoted her life to the idea that the immune system played a key part in her father’s discovery and that there was more to learn – perhaps even a cancer cure to discover.
1953
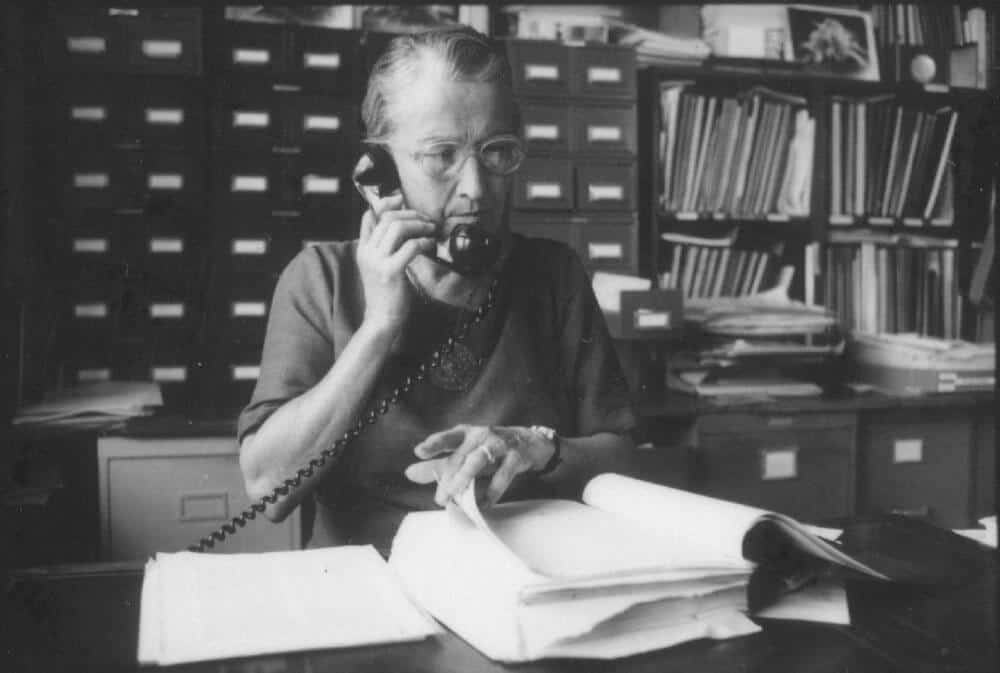
Helen Coley Nauts Challenges Cancer Treatment Orthodoxy
In addition to educating herself in the disciplines of oncology and immunology, Helen Coley Nauts distinguishes herself as a meticulous record keeper who interpreted and published the life’s work of her father, Dr. William B. Coley. The data compilations, published in a series of monographs detailing long-term patient responses to her father’s treatment, were so exact that they are consulted by cancer researchers to this day.
1959
Mice Demonstrate Resistance to Tumor Growth
In 1959, Drs. Lloyd J. Old, Donald A. Clarke, and Baruj Benaceraff publish a paper detailing how mice injected with Bacillus Calmette-Guerin (BCG), a type of bacterial immunotherapy similar to Dr. William B. Coley’s mixed bacterial toxin, increases resistance to tumor growth. More than 30 years after their initial discovery, and with funding from CRI granted to Dr. Alvaro Morales, in 1990 BCG became the first active immunotherapy approved by the FDA for the treatment of cancer, in this instance superficial (non-invasive) bladder cancer, which continues to be a standard, effective treatment.
1960s
Immunology and Cancer Biology Spawn the New Field of Tumor Immunology
1960
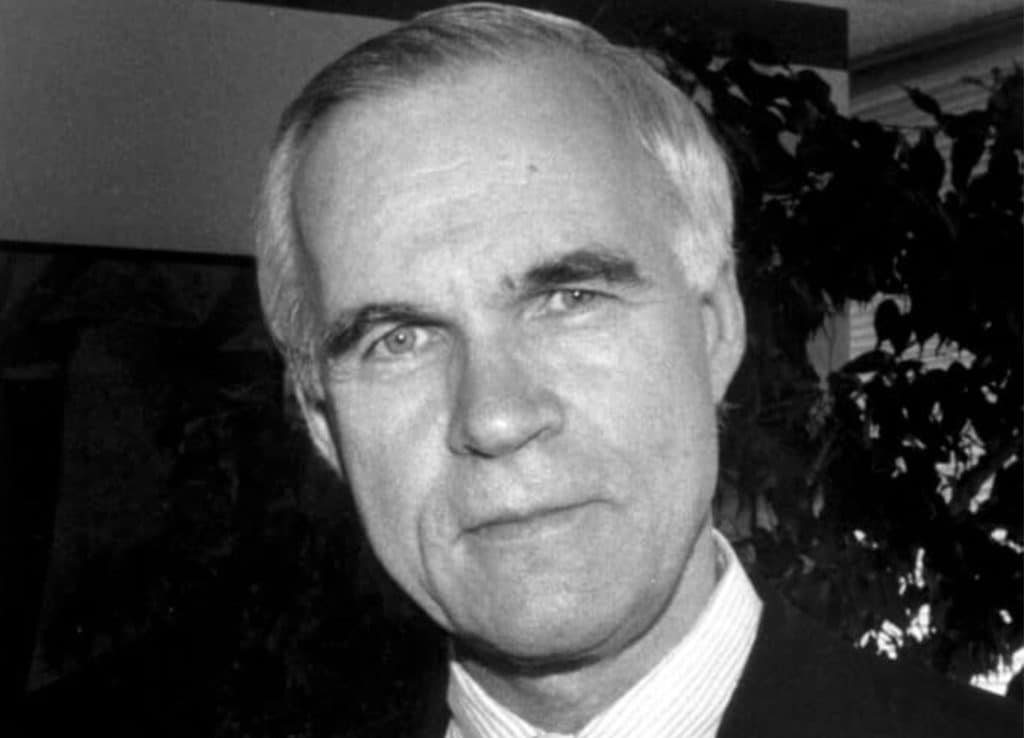
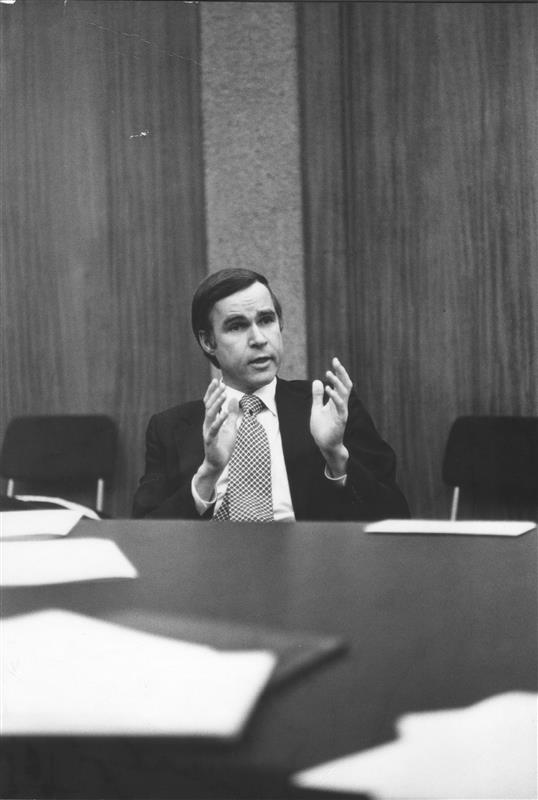
Dr. Lloyd J. Old Turns His Scientific Genius to Cancer Immunotherapy
During the 1960s, Dr. Lloyd J. Old makes several discoveries helping him to realize his goal of establishing a solid foundation for the field of tumor immunology – including the mechanisms behind how Dr. Coley’s bacterial toxins may have initiated anti-cancer immune responses and how the immune system recognizes threats including cancer. Cancer immunology would remain his lifelong passion.

1967
CRI Funds Dr. Lloyd J. Old’s Groundbreaking Research
CRI begins funding the research of Dr. Lloyd J. Old and his colleagues, which results in some of the earliest data demonstrating that the immune systems in mice could be activated to reject transplanted tumors – providing proof that the immune system recognizes and can eliminate cancer. Their work would inform later clinical studies in humans.
1968
Surface Markers on Immune Cells Identified
A revolutionary idea at the time, different types of immune cells and their functions can be identified by distinct markers of the surfaces of their cells. Dr. Lloyd J. Old and colleagues are the first to characterize a cell-surface marker known today as CD8 that signals cytotoxic, or ‘killer’ T cells, while another cell surface marker known today as CD4 defines ‘helper’ T cells, both essential to mounting an effective immune response to cancer.
1970s
Establishing Tumor Immunology as a Scientific Discipline
1971
CRI Launches Its Postdoctoral Fellowship Program to Seed the Field of Tumor Immunology
Dr. Lloyd J. Old takes the helm as CRI’s scientific and medical director and establishes CRI’s Postdoctoral Fellowship Program. His aim is to produce a new generation of immunologists capable of building the immunotherapy field from the ground up. Dr. Old’s vision bore out. Guided by a review committee chaired for many years also by Dr. Carl F. Nathan and then Dr. Ellen Puré, CRI has funded over 1,500 postdoctoral fellows, almost all of whom have made important discoveries and now mentor new generations of tumor immunologists.
1976
Dr. Rolf Kiessling Helps Identify Natural Killer Cells
Dr. Rolf Kiessling (pictured), along with Dr. Klas Kärre, contribute to the discovery and characterization of natural killer cells while Kiessling is a postdoctoral fellow in the laboratory of Dr. Eva Klein at the Karolinska Institute in Sweden.
1976/79
Natural Immune Response to Cancer Identified in Patients
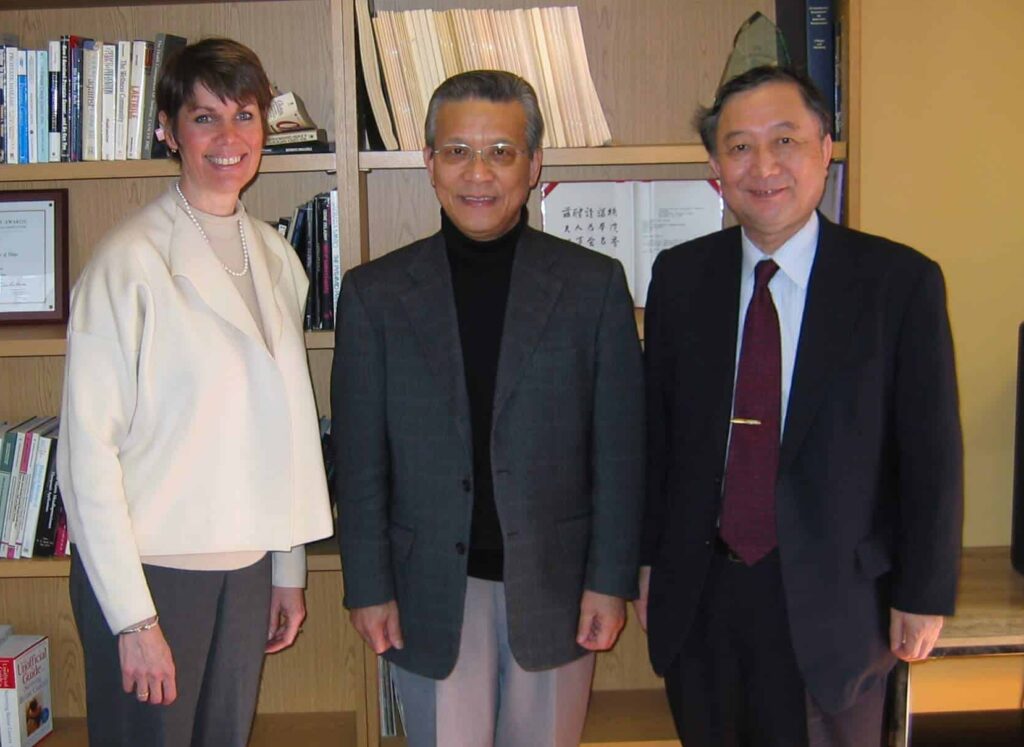
Drs. Lloyd J. Old, CRI postdoctoral fellow Hiroshi Shiku, and CRI grant recipient Herbert Oettgen make breakthrough discoveries in the late 1970s, including the discovery of naturally produced cancer-targeting antibodies in the blood of cancer patients. These discoveries confirm that the human immune system can recognize and target cancer. Here, Dr. Shiku (center) poses with CRI CEO Dr. Jill O’Donnell-Tormey and a colleague in 2006.
1980s
Visualizing T Cell Targets
1983
T Cell Antigen Receptor Identified
The T cell receptor, which binds to the MHC-antigen structure mentioned below, is critical to T cells’ ability to recognize abnormal markers associated with threats – and destroy the cells that display them, including cancer cells. This discovery is made by Drs. James P. Allison, Philippa Marrack, John Kappler, and their colleagues, and makes possible the development of lifesaving immunotherapies available today.

1983
A New Immune System Sentinel Discovered: The Dendritic Cell
Drs. Ralph Steinman and Jonathan Austin discover that dendritic cells foster T cell growth and adaptive immune responses, opening entirely new therapeutic avenues leading to the first FDA approval of an active immunotherapy (Dendreon’s Provenge for prostate cancer) and Dr. Steinman being awarded the Nobel Prize in 2011.
1986
CRI Launches Its Investigator Award Program to Power Research in Tumor Immunology
CRI establishes its Investigator Award Program to address the growing need for funding among more experienced scientists in need of support for their newly-established laboratories, including Dr. Thomas Gajewski, today a prominent professor and medical doctor at the University of Chicago, as well as hundreds of other tumor immunologists who credit CRI with providing critical funding when other organizations would not.

1987
MHC Antigen Complex Structure Discovered
Two CRI-funded groups – one involving Drs. Pamela Bjorkman (pictured), Don Wiley, and Jack Strominger, and another with Drs. Marcia Blackman, Phillipa Marrack, and John Kappler – discover how T cell receptors bind to antigens presented via major histocompatibility complex (MHC) molecules and determine whether a cell is normal. In 1987, an X-ray crystallography ‘image’ of an MHC cradling an antigen clarified how our body’s T cells surveil and identify cancer cells.
1987
Dr. Susumu Tonegawa Wins the Nobel Prize
With CRI support, 1987 Nobel Prize Laureate Dr. Susumu Tonegawa decodes how the immune system produces a randomly diverse repertoire of antibodies capable of identifying and targeting a near-infinite number of potential threats including cancer, viruses, bacteria, and parasites.
1990s
Convening the Field and Fostering Collaboration
1991
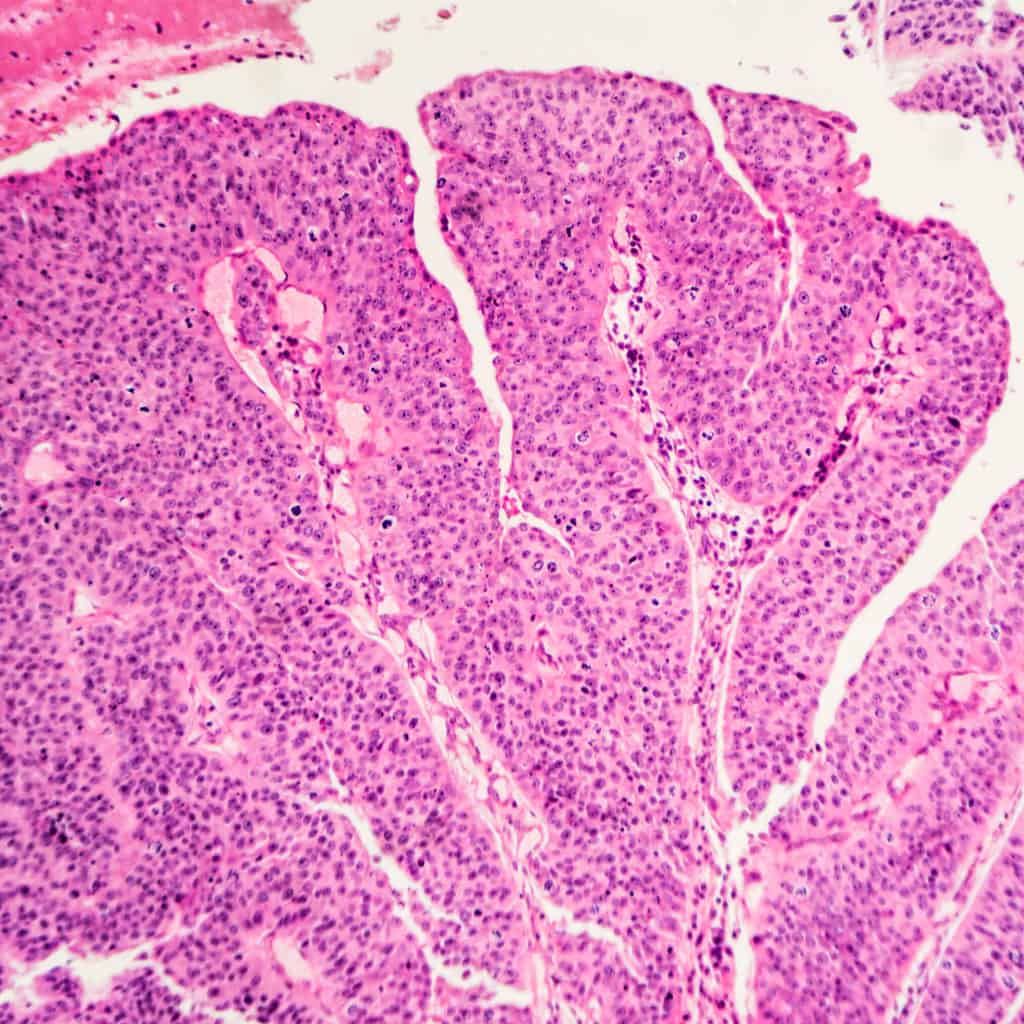
First Tumor-Associated Antigen Discovered
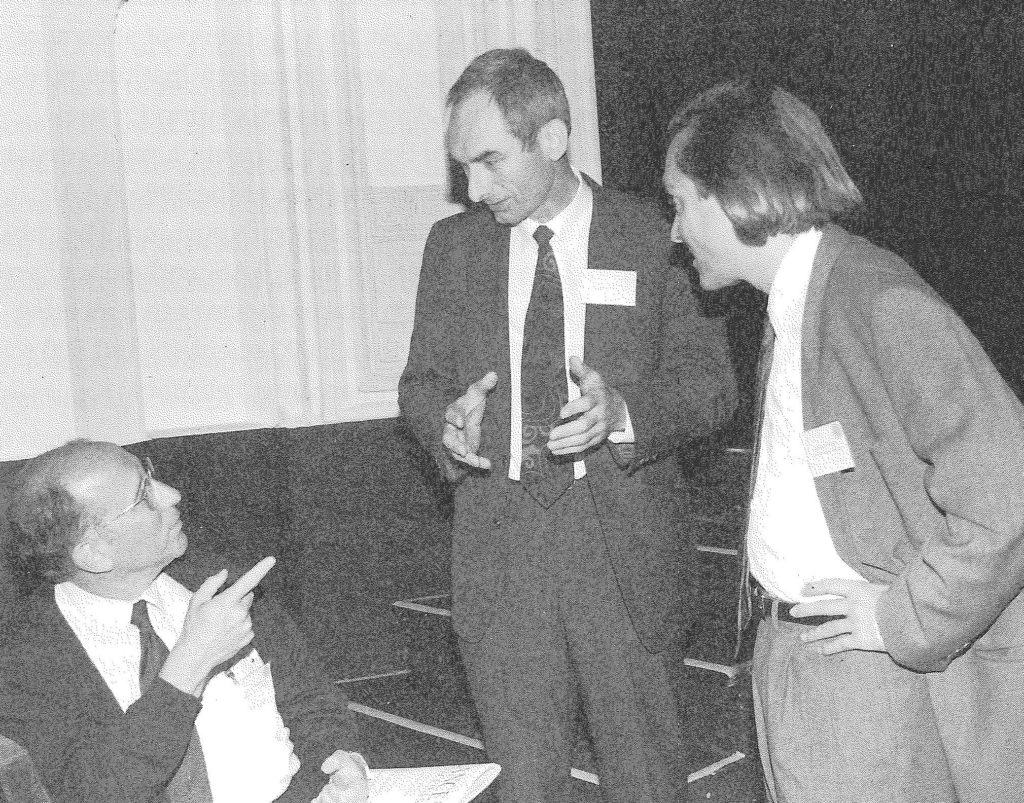
CRI-funded Dr. Alexander Knuth (right) along with Dr. Thierry Boon (left) identify melanoma-associated antigen (MAGE), the first-ever discovery of a tumor-associated antigen. This solves one of the oldest mysteries in tumor immunology – the so-called ‘needle in a haystack’ that enables the immune system’s T cells to recognize cancer cells.
1994
CRI Launches Its Annual Cancer Immunotherapy Symposium to Provide a Forum for the Field
By the 1990s, there is an appetite for establishing a formal network of cancer immunology’s global talent – birthing CRI’s Annual International Cancer Immunotherapy Symposium in 1994. These annual meetings host hundreds of researchers from dozens of countries to discuss data from the emerging field of tumor immunology and provided an opportunity for these scientists to forge new research collaborations that have produced other key advances in the field. (From left to right: Drs. Steven A. Rosenberg, Hans Schreiber, and Nicolas Restifo at the 1994 CRI International Cancer Immunotherapy Symposium.)

1994
Drs. Arlene Sharpe and Frank Borriello Describe How the Immune System Prevents Autoimmunity
Dr. Arlene Sharpe, who mentored CRI postdoctoral fellow Dr. Frank Boriello, and colleagues discover that the CTLA-4 pathway acts as a brake on T cells. They engineer mice without CTLA-4 receptors, recording their chaotic immune responses that harm healthy tissues and organs. Their work, along with that of Dr. James P. Allison, directly led to the first FDA-approved checkpoint immunotherapy ipilimumab 17 years later.
2000s
Immunotherapy Enters a Renaissance

2001
Dr. Robert D. Schreiber Proves the Human Immune System Sees and Shapes Cancer
CRI grantee and associate director of CRI’s Scientific Advisory Council Dr. Robert D. Schreiber along with Dr. Lloyd J. Old and other CRI-funded scientists reignite interest in cancer immunotherapy by demonstrating that mice engineered without elements of a functioning immune system saw a higher rate of cancer. This overturns prior conclusions about immunotherapy’s potential and empirically proves that the immune system plays a role in eliminating cancer. This work also demonstrates how the immune system affects cancer development via a process called “immuno-editing.”

2001
CRI Launches the Cancer Vaccine Collaborative to Advance Immunological Insights into Patient Responses to Treatment with Immunotherapy
CRI and the Ludwig Institute for Cancer Research join forces to establish the Cancer Vaccine Collaborative (CVC), a coordinated academic research program to develop therapeutic vaccines for the treatment of cancer. Viewed as a “missing link” in biomedical research, the CVC is the first network of its kind in immuno-oncology to bridge the divide between hypothesis-based investigation in academic laboratories and drug development in the pharmaceutical industry.

2002
CRI Forms the Cancer Immunotherapy Consortium to Shape a Shared Vision for the Field and Harmonize Methods to Aid IO Development
CRI convenes the Cancer Immunotherapy Consortium (CIC), an international “think tank” through which stakeholders from academia, industry, regulatory bodies, and the cancer patient community come together to tackle topics of key importance to the clinical development of cancer immunotherapies. Through annual workshops and collaborative research efforts, the CIC, chaired by CRI Scientific Advisory Council Member Dr. Axel Hoos, produces a series of publications and resources designed to harmonize efforts across the field to ensure reliable interpretation of clinical research data.
2006
Revitalizing ‘Exhausted’ T Cells
Drs. E. John Wherry and David Masopust, both CRI-funded fellows in the lab of Dr. Rafi Ahmed demonstrate that by blocking the PD-1 immune checkpoint’s receptor activity, ‘exhausted’ T cells could be revitalized, increasing their ability to destroy virus-infected cells. This novel approach proves effective against cancer, empowering the development of various PD-1/PD-L1 checkpoint immunotherapies now treating millions of cancer patients each year.

2006
FDA Approves First Vaccine to Prevent Infection with the Cancer-Causing Human Papillomavirus (HPV)
After the development of virus-like particle technology by CRI-funded scientist Dr. Ian Frazer and colleagues, the vaccine Gardasil is approved by the FDA for the prevention of several types of cancers associated with infection by sexually-transmitted human papillomavirus (HPV). The vaccine is 90 percent effective at preventing infection by cancer-associated strains of HPV, resulting in dramatic drops in the incidence of HPV-associated cancers worldwide. In the wake of this revolutionary vaccine technology, Dr. Frazer is named “2006 Australian of the Year.”
2007
CRI and The Irvington Institute for Immunological Research Join Forces
The Irvington Institute for Immunological Research — long a source of vital funding for young scientists in immunology — merges with CRI, combining the two organizations’ postdoctoral fellowship programs and consolidating their resources and board leadership to increase funding of young, exceptionally talented scientists in the fields of immunology and tumor immunology. The resulting CRI Irvington Postdoctoral Fellowship Program is able to grow the number of annually funded fellows by 25 percent, helping more young scientists establish careers in academic research and discovery. (Pictured: Jacob Yount, PhD, 2007 CRI Fellow)
2010s
Immunotherapy Revolutionizes Cancer Treatment for Millions of Cancer Patients
2011
First Checkpoint Inhibitor Approved
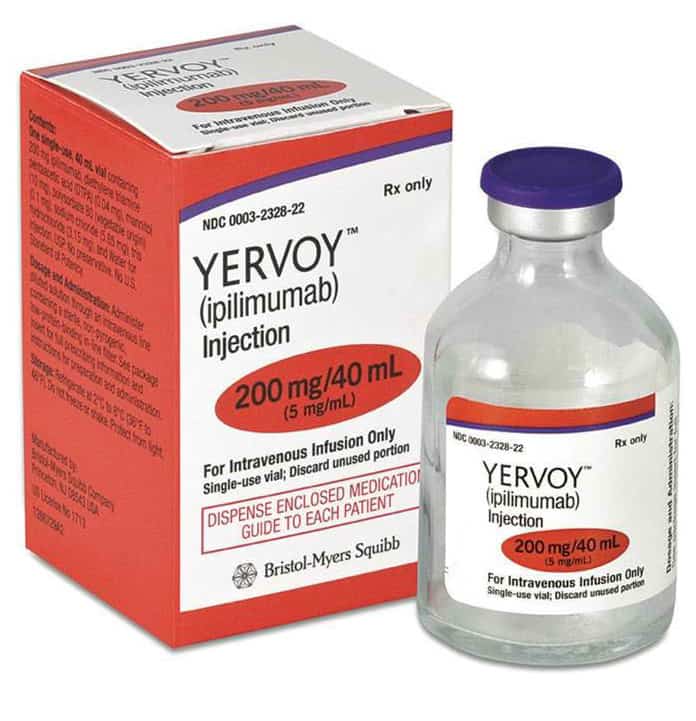
Dr. James P. Allison discovers how to circumvent the immune system’s braking mechanisms with his revelation of how the CTLA-4 receptor on the immune system’s T cells shuts down attacks against cancer cells. Clinical trials testing anti-CTLA-4 antibodies in patients with melanoma demonstrate greater benefit to patients, leading to the FDA approval of ipilimumab (Bristol Myers Squibb’s Yervoy). CRI Clinical Director Dr. Jedd D. Wolchok contributes to the pivotal phase 3 study leading to the FDA approval.

2011
CRI’s Scientific Leadership Changes Hands
Dr. James P. Allison is appointed director of the CRI Scientific Advisory Council following the retirement of Dr. Lloyd J. Old after his forty years of service to CRI and the field of tumor immunology — service which earns Dr. Old the title, “Father of Modern Tumor Immunology.” The change in scientific leadership ushers in a new era of programmatic evolution focused on the clinical translation of laboratory discovery into lifesaving immunotherapies — modeled after Dr. Allison’s research breakthrough and dogged persistence to move his discovery into clinical development.
2012
CRI Launches the Anna-Maria Kellen Clinical Accelerator and Venture Fund
Following the foundational work conducted by the CRI-LICR Cancer Vaccine Collaborative, CRI evolves its clinical research program to establish collaborative relationships across academia and industry, gaining access to highly promising immunotherapies and designing clinical trials testing novel combination approaches across a variety of cancer types. Under the direction of CRI Scientific Advisory Council Associate Director and CRI Clinical Director Dr. Jedd D. Wolchok, the Clinical Accelerator expands its clinical trial management partnerships, grows its access to novel immunotherapies, and designs promising trials that are innovative and non-duplicative of industry efforts. The program is powered by a philanthropic Venture Fund structured to fuel future research from milestone-based returns on investment.

2012
The CRI Clinic and Laboratory Integration Program Is Launched to Bridge Bench Discovery and Insights from Patient Responses to Immunotherapy
With the pace of both laboratory and clinical discovery in cancer immunology and immunotherapy rapidly increasing, CRI launches its Clinic and Laboratory Integration Program (CLIP), which provides catalytic support for the translation of basic discoveries into novel therapies that can be tested in patients and for bringing questions from clinical studies back to the lab for deeper interrogation in hope of leading to novel treatment strategies that can be taken back into the clinic.

2013
Immunotherapy Named “Breakthrough of the Year”
The academic journal Science names cancer immunotherapy “Breakthrough of the Year” in the face of remarkable recoveries and improved patient survival in cancer patients. Several years later, the American Society of Clinical Oncology (ASCO) would also laud immunotherapy’s potential to transform cancer treatment for two consecutive years.

2013
CRI Raises Awareness for Immuno-Oncology with the First Annual Cancer Immunotherapy Month
CRI organizes the first Cancer Immunotherapy Month (CIM), held each June, to raise awareness of the lifesaving potential of cancer immunotherapy and to call attention to the urgent need for continued funding of basic research to drive new discoveries. CIM invites individuals, companies and their employees as well as nonprofit partners and organizations and their members to join in the global social media campaign by wearing white to symbolize the white blood cells of the immune system and the white lab coats of doctors and scientists working daily to create a world #Immune2Cancer.

2014
Predictive Biomarkers that Guide Cancer Patient Treatment Identified
CRI Investigator and, later, CRI Scientific Advisory Council Member Dr. Antoni Ribas, an immunologist at the University of California, Los Angeles, identifies patient traits that can predict their responses to checkpoint blockade immunotherapy. This work helps oncologists to determine optimal treatment courses for patients, such as avoiding predictably ineffective treatments or prescribing treatments more likely to help. This groundbreaking work spares patients from unnecessary treatments, saving precious time and informing better treatment plans.
2015
Genetic Engineering Unleashes New Powers of the Immune System
Dr. Alexander Marson successfully unlocks genome editing to decode and rewire the human immune system genetically to enact progress in T cell cancer immunotherapy. His innovative work later earns him a CRI Lloyd J. Old STAR grant, enabling him to push scientific discovery in cancer immunology into new and unexpected but beneficial directions.

2015
Second Checkpoint Inhibitor Approved, Expanding Immunotherapy’s Benefit to More Patients
The immunotherapy pembrolizumab (Merck’s Keytruda), in combination with radiation, helps former United States President Jimmy Carter recover from metastatic melanoma, a deadly type of skin cancer that had spread to his brain. A few years prior to advances in cancer immunotherapy, this cancer would have been terminally untreatable.

2016
CRI Launches Its First Immunotherapy Patient Summit Connecting Patients and Caregivers to IO Experts and Clinical Trials
As immunotherapy becomes increasingly part of the standard of care or an option in clinical trials for patients, CRI as the trusted source of IO information establishes the first-of-its-kind conference bringing patients and caregivers together with immunotherapy expert doctors as well as other cancer patients treated with immunotherapy to learn what immunotherapy is and how it works, how to access clinical trials, and what to expect from the patient experience. The program empowers people to ask their doctors about immunotherapy and equips them with the knowledge to do so as informed patients. (Left to right: MaryElizabeth Williams, Stephen Estrada, Ariella Chivil, and Donna Fernandez)

2016
U.S. Government’s “Cancer Moonshot” Places Immunotherapy at the Core of Its Strategy to Reduce Cancer Deaths
Then-Vice President Joseph Biden launches the Cancer Moonshot to hasten the rate of scientific progress against cancer. Immunotherapy is a keystone of this initiative. CRI CEO Dr. Jill O’Donnell-Tormey participates in advisory panel discussions that inform the Moonshot’s research strategy and public rollout.
2017
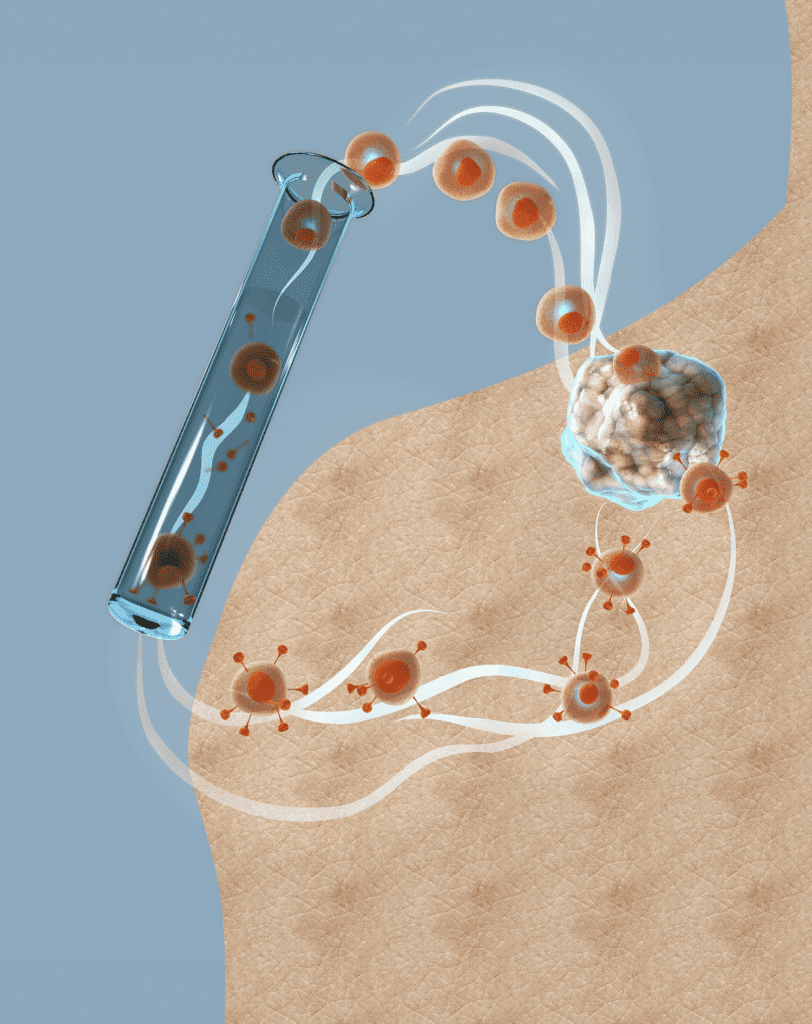
The Era of CAR T Cell Immunotherapy Begins
The FDA approves the first CAR T cell therapy, using immune cells from patients that are genetically reengineered to attack cancer-causing cells, resulting in very high cure rates for blood cancers. The confluence of gene engineering technology, immuno-biology, and cancer biology sparks an entirely new approach to harnessing the body’s immune system to fight cancer.
2017
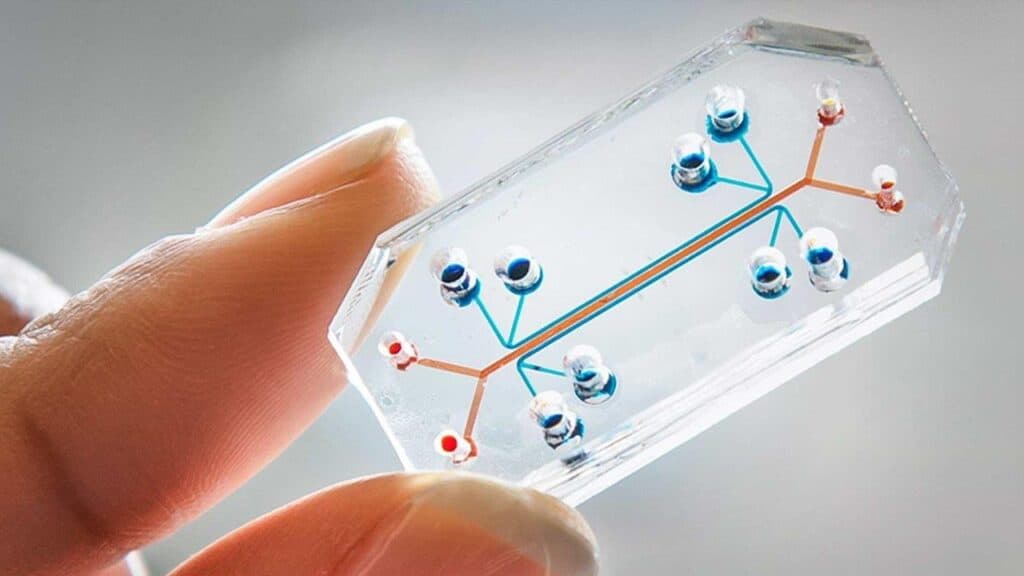
CRI Launches Its Technology Impact Award Program to Power Transformative Collaborations Leading to New Tech and Tools to Speed IO Discovery
CRI’s Technology Impact Award addresses the gap between technology development and the clinical application of cancer immunotherapies. The program provides seed funding that allows technology developers and clinical cancer immunologists to collaborate and create novel platform technologies in bioinformatics, modeling systems, immunological and tumor profiling tools, and other relevant technologies that facilitate deeper insights into the mechanisms of action of cancer immunotherapies.

2018
Dr. James P. Allison Wins the Nobel Prize in Physiology or Medicine
For his breakthrough discovery of how to unleash the immune system to attack cancer via immune checkpoint blockade, CRI Scientific Advisory Council Director Dr. James P. Allison wins the Nobel Prize. His discoveries lead to the first effective approved active immunotherapy for cancer (Yervoy, FDA-approved in 2011) and opened the way for other immune checkpoint-blocking antibodies that follow.

2019
CRI Launches the CRI Lloyd J. Old STAR Program to Free Today’s IO Stars to Explore New Research Directions
One of CRI’s boldest and most ambitious grant programs, the Lloyd J. Old STAR Program (Scientists TAking Risks), provides $1.25 million grants to individual, highly-accomplished, mid-career scientists that are not tied to a specific research project, but rather aims to provide a degree of flexibility and freedom to explore outside-the-box and disruptive avenues of research. STARs are expected to be future “stars” in the field of cancer immunology.
2020s
CRI Reaches New Communities with Accessible Information and Helps Stave a Global Pandemic
2021
CRI Commits to Furthering Diversity and Inclusion in Academic Research and Patient Care
CRI-Bristol Myers Squibb Fellow Dr. Ryan K. Alexander is one of the first fellows funded through CRI’s Postdoctoral Fellowship to Promote Racial Diversity, a program that CRI initiated to overcome racial and ethnic disparities in academic support for talented scientists in immunology and tumor immunology. Dr. Alexander explores nanobody-based technologies to enhance CAR T cell therapy responses in patients with pancreatic cancer.
2021
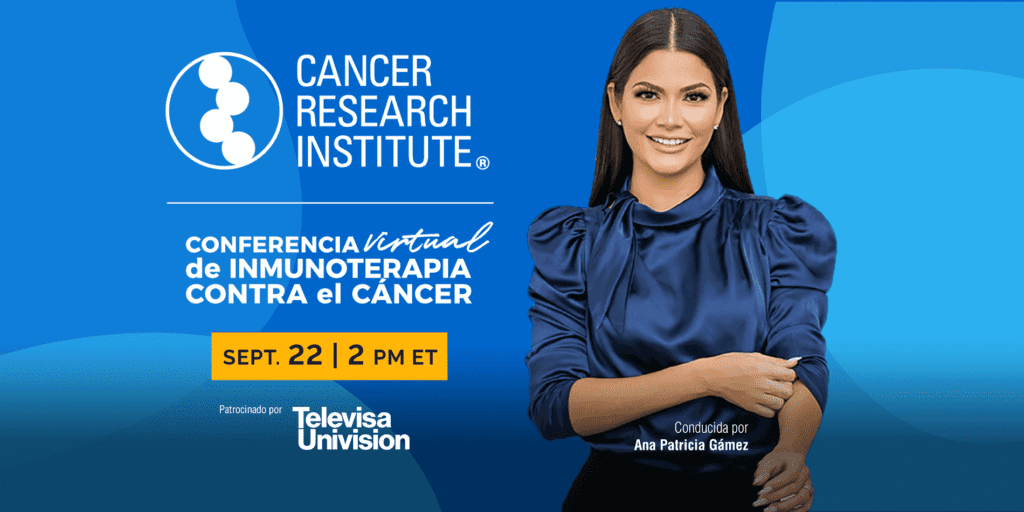
CRI Launches Spanish-Language Immunotherapy Patient Summit and Clinical Trial Finder and Translates Its Website into Spanish
Language is a barrier that can impede Spanish-speaking patients or caregivers while navigating a cancer diagnosis and treatment plan when most available information is presented only in English. To address this, CRI launches a Spanish-language version of its website and clinical trial finder service and pilots its first-ever all-Spanish-language Virtual Immunotherapy Patient Summit. These resources help Spanish-speaking people access potentially lifesaving information about cancer immunotherapy and clinical trials.

2021
Drs. Ugur Sahin and Özlem Türeci Halt COVID’s Devastation with CRI-Funded Vaccine Research
While the COVID-19 pandemic claims millions of lives worldwide, BioNTech’s Drs. Ugur Sahin (right) and ÖzlemTüreci (left) develop the Pfizer-BioNTech COVID-19 mRNA vaccine, one of the first effective vaccines to prevent severe COVID-19 complications following infection with the novel coronavirus. This astonishingly fast response to a global pandemic saves millions of people’s lives. This earns them CRI’s prestigious William B. Coley Award for Distinguished Research in Basic and Tumor Immunology in 2021, along with Drs. Katalin Karikó and Drew Weissman, whose body of work contributed to effective mRNA vaccine technology.

2022
A New Checkpoint Inhibitor Immunotherapy Receives FDA Approval, Further Expanding Immunotherapy’s Potential to Save Lives
The FDA approves Bristol Myers Squibb’s relatlimab (anti-LAG-3 checkpoint blockade), in combination with nivolumab (anti-PD-1 checkpoint blockade), as the drug combo Opdualag, to treat melanoma, the first FDA approval of a checkpoint other than those targeting the CTLA-4 or PD-1/L1 pathways and the first new immune checkpoint-targeting immunotherapy approved since late 2014.

2022
CRI Launches New Funding Programs in Data Sciences and Bioinformatics to Equip Today’s Young Scientists with Knowledge Needed to Succeed in a Data-Rich Future in Immuno-Oncology
CRI’s Scientific Advisory Council guides CRI’s launch of new funding initiatives designed to train new generations of immunologists and tumor immunologists in bioinformatic data science and computational analysis, necessary skills for success in the rapidly evolving field of tumor immunology.