Accelerating Clinical Trial Discoveries Toward Better Patient Care
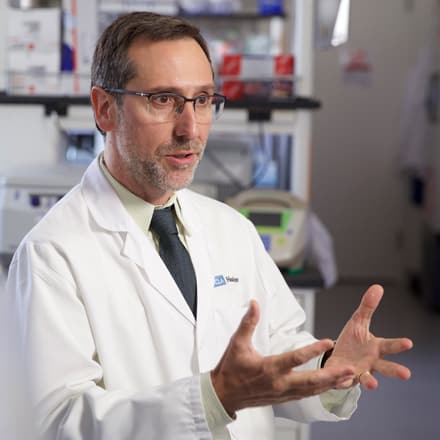
In the world of cancer immunotherapy, Antoni Ribas, MD, PhD, has earned a reputation for being both a world-class scientist and a devoted physician. As a tumor immunologist at UCLA’s Jonsson Comprehensive Cancer Center, Dr. Ribas specializes in the research and treatment of melanoma, the deadliest form of skin cancer. He is conducting several large clinical trials of cutting-edge treatments, including both immunotherapies and targeted therapies.
Dr. Ribas is the principal investigator for a large phase 1 trial of the anti-PD-1 drug pembrolizumab, owned by Merck. Pembrolizumab (MK-3475) belongs to the class of drugs known as checkpoint inhibitors. By binding to and blocking certain molecules on T cells, in this case a molecule called PD-1, pembrolizumab “takes the brakes off” the immune response, allowing a more powerful response to cancer.
Dr. Ribas presented preliminary results of this trial at the May 30–June 3, 2014 meeting of the American Society for Clinical Oncology (ASCO). For the 411 melanoma patients enrolled in the trial, the 1-year overall survival rate was 69%—almost three times better than with standard therapy. Results like these have raised high hopes for immunotherapies targeting the PD-1 pathway.
Dr. Ribas is a member of the Cancer Research Institute (CRI) clinical trials network, as well as the CRI/Stand Up to Cancer “Dream Team.” We spoke with Dr. Ribas about what it’s like to be a tumor immunologist at this exciting time.
When did you first experience the power of immunotherapy to treat cancer?
Dr. Ribas: About 11 years ago, I had a patient with a bad melanoma, a mucosal melanoma. He had just gone through surgery, gone through biochemotherapy—that’s getting three chemotherapy drugs and two immunotherapy drugs, IL-2 and interferon—and requires being a week in the hospital and is probably the most toxic thing that oncologists have learned how to do. And he kept just blowing through it; his tumor was continuing to grow and there were multiple subcutaneous lesions, liver lesions, peritoneal metastases. It was just bad. And, honestly, I hadn’t seen anything work in this situation.
We started him on tremelimumab [an anti-CTLA-4 antibody developed by Pfizer, now owned by MedImmune] and not very long afterward he started saying that some of the skin lesions were going away. And I thought, “Oh, you have such a bad melanoma, it’s too soon to even think about being happy about that.”
And then we did a set of scans and they were all a bit confusing. We didn’t really know what was happening, which often happens with immunotherapy. At the beginning, it’s not clear if there’s a benefit or not. But then after that he had a new set of scans and I remember going into the radiology room and the radiologist saying, “I don’t know what you did, but this is not melanoma.”
At that time, we had nothing that actually gave any responses. I don’t think that the radiologist had ever seen a melanoma respond to anything. But here his scan showed that his liver mets were decreased, the peritoneal carcinomatosis was disappearing…it was just amazing. And of course, we didn’t know it at that time, but it looks like the patient has been cured. It’s 10 years later and the cancer has never come back.
Can you talk a little bit about what it was like to treat patients before these new therapies existed?
Dr. Ribas: Before this, there were occasionally patients made well with IL-2 [interleukin-2]. But it was the patients with the least aggressive melanomas who were doing the best with IL-2. For a patient with very advanced disease, these therapies had little to no chance to work. We’re talking about 10 years ago. And then you would hear about a patient occasionally who did well with high-dose IL-2, or with CTLA-4 blockade, but the reports were in a minority of patients. But now, it’s become a much more common thing because of the advent of the PD-1 and PD-L1 antibodies. We’re seeing a lot of these patients with very impressive immune-mediated responses, even with advanced disease.
Were you surprised by this change?
Dr. Ribas: We obviously knew that the immune system could lead to durable responses in patients with cancer and you could model it in animal models. But doing it reproducibly in patients was a different story. The big conceptual changes were when we started taking brakes off the immune system, first with anti-CTLA-4 and then anti-PD-1. That’s when we were able to see this ability of the immune system to really go against the cancer.
Let’s talk about the PD-1 antibodies for a bit. There are different PD-1 and PD-L1 antibodies out there, owned by different companies. Do we know anything about how these drugs are different?
Dr. Ribas: Well, they are all different molecules. They are antibodies, but they have different antibody backbones and they bind to different parts of PD-1 or PD-L1. But actually, different anti-PD-1 and anti-PD-L1 antibodies are equally giving unprecedented levels of durable responses. So if there are differences, they’ll be figured out in the future, but what makes the big difference now is that they’re all active, and they are active in a significant number of patients.
Do you have a sense of how soon a PD-1 antibody will be approved?
Dr. Ribas: Yes, it seems to be that the one from Merck [pembrolizumab] is in advanced approval process for melanoma, and the one from BMS [nivolumab] for lung cancer will probably follow. So we’re doing really well. It hasn’t been too long that we started using them.
When did you know you wanted to become a tumor immunologist?
Dr. Ribas: It was not an easy thing to do. For a while, people were not keen on anyone who wanted to do tumor immunology. So, 18 years ago, I finished my training in Spain. I was a medical oncologist and I was treating patients with lymphoma and breast cancer. Chemotherapy would give some good responses and I was excited about that. But I wanted to learn something new and I wanted to understand the mechanism of things. So I applied to do a postdoc in a tumor immunologist’s lab at UCLA. And I told my wife that we would go for a year or two and I would do some laboratory research. Many of my friends in Spain discouraged me. They said, “Why are you going to do tumor immunology? You should be doing targeted therapy.” That was back when Herceptin was being developed.
So I went. I liked what I was doing. It’s been 18 years and we haven’t gone back.
You mentioned targeted therapies. Are there any trials out there now that are combining PD-1 antibodies with, say, a B-raf inhibitor?
Dr. Ribas: Yes. We started doing that. We actually have two clinical trials that are combining B-raf and MEK inhibitors and the PD-1 or PD-L1 antibodies. It is just starting. It’s based on solid data and I hope we’ll make a big difference because if we can merge the high response rate and the elegance of targeted therapy with the durability of responses from immunotherapy, I feel we will make a big difference in treating cancer.
Why did you decide to do an MD/PhD instead of just an MD or a PhD alone?
Dr. Ribas: I wanted to understand how things work and why they work. To be able to understand biology and bring it to patients—that is what I had an interest in.