Immunotherapy Treatment Types
Wherever you are on your cancer treatment journey, you may want information on the types of immunotherapy available today.
Here we describe some of the different approaches to cancer immunotherapy and how they are used to treat a wide variety of cancers. Please note that these treatments do not include all cancer immunotherapies currently available, but represent some promising approaches that are currently approved by the FDA or being tested in clinical trials.
Immunotherapy, a cutting-edge approach to cancer treatment, encompasses a diverse array of innovative strategies, each meticulously engineered to rally the body’s own immune defenses in the relentless battle against cancer.
These novel therapies represent a transformative frontier in the landscape of cancer treatment. Explore the multifaceted world of immunotherapy and unveil the distinct forms it takes and the pivotal roles it plays in combating a vast spectrum of cancer types.
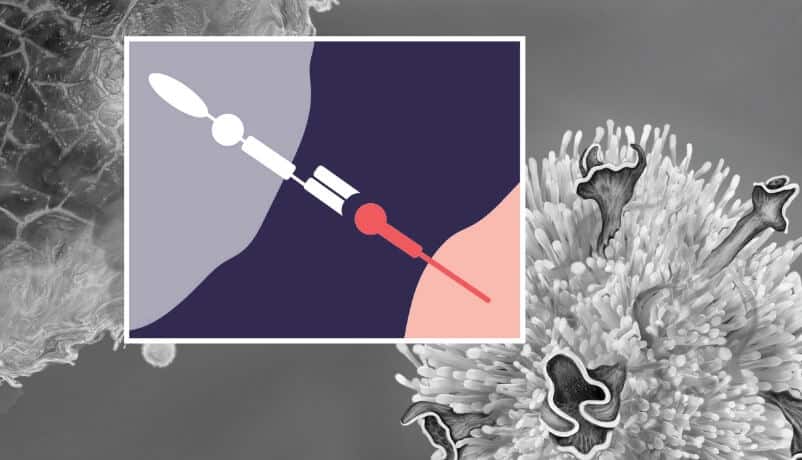
Adoptive Cell Therapy
Adoptive cell therapy is a type of cancer treatment that reactivates, enhances, and expands naturally occurring, cancer-fighting immune cells…

Cancer Vaccines
Preventive vaccines can protect against cancer development, whereas therapeutic vaccines can stimulate immune responses against existing tumors.
Immunomodulators
Immunomodulators are a form of immunotherapy that manipulate the “gas pedals” and “brakes” of the immune system to fight…

Oncolytic Virus Therapy
Oncolytic virus therapy uses modified viruses that can infect and destroy tumor cells.

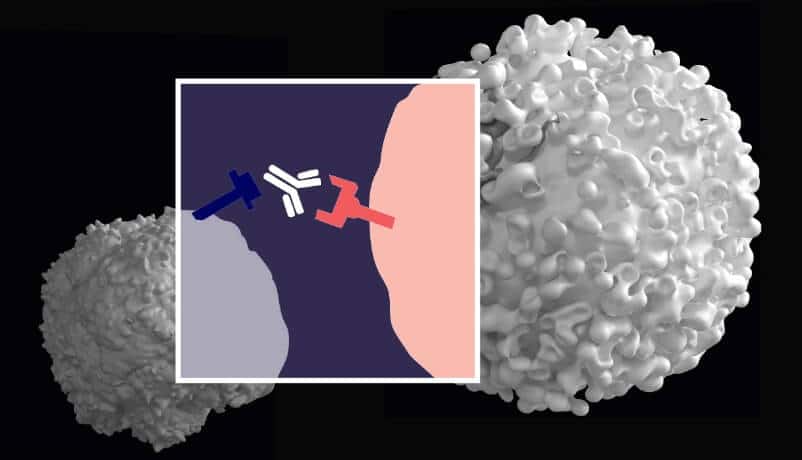
Targeted Antibodies
Targeted antibodies are a type of immunotherapy that can disrupt cancer cell activity and alert the immune system to…
Explore Immunotherapy Treatment Types
What types of cancer does immunotherapy treat?
Immunotherapy has shown remarkable success in treating advanced cases of cancers like lung cancer, melanoma, advanced bladder, and kidney cancer, amongst others. It’s important to note that the list of cancers treatable with immunotherapy continues to grow as more drugs undergo clinical trials.
From preventive vaccines for cervical and liver cancer to extending the lives of those with metastatic melanoma, immunotherapy research has produced groundbreaking advancements in treating an ever-expanding list of cancer types.
The response to immunotherapy in cancer treatment is influenced by various factors. Tumor type and tumor intrinsic characteristics such as mutational burden, PD-L1 expression, and tumor microenvironment can impact response rates. The patient’s own immune system, prior treatments, genetic factors, overall health, and combination therapies also play vital roles. Emerging research also suggests a connection between the gut microbiome and immunotherapy response. Predicting individual responses remains complex, and personalized treatment recommendations are made by a medical team considering these diverse factors.
Eligibility for these therapies typically depends on previous treatment attempts or specific tumor markers. However, it’s crucial to consult your healthcare provider for personalized guidance on immunotherapy eligibility and to address any specific medical inquiries or concerns.
Cellular Immunotherapies: Harnessing the Power of Immune Cells
Cellular immunotherapies, often referred to as “living drugs,” represent a paradigm shift in cancer treatment. This approach leverages the body’s own immune system to fight cancer by manipulating and reprogramming immune cells. Advances in gene-editing technologies like CRISPR have greatly facilitated the development of these therapies, making it more feasible to engineer immune cells to target cancer. Among these cells, killer T cells are particularly adept at recognizing and targeting cancer cells. Various modalities of this innovative therapy include:
- Tumor-Infiltrating Lymphocyte (TIL) Therapy: TILs are harvested from the patient, multiplied in number, and then reintroduced into the body to target the cancer.
- Engineered T Cell Receptor (TCR) Therapy: Immune cells are genetically modified to enhance their cancer-fighting capabilities.
- Chimeric Antigen Receptor (CAR) T Cell Therapy: CAR T cells are custom-designed to recognize specific cancer markers.
- Natural Killer (NK) Cell Therapy: NK cells are activated to attack cancer cells.
These therapies are continually evolving and have been utilized in clinical trials for treating cancers such as lymphoma, leukemia, and certain solid tumors like glioblastoma.
Cancer Vaccines: Boosting the Immune System’s Vigilance
Cancer vaccines are a form of immunotherapy that educates the immune system about cancer cells, enabling it to recognize and destroy them. While traditional vaccines protect against infectious diseases, cancer vaccines work by exposing the immune system to cancer-specific antigens. They can be categorized into:
- Preventive Cancer Vaccines: These vaccines protect against infections that can lead to cancer. For instance, the Human Papillomavirus (HPV) vaccine is designed to protect against the strains of HPV most commonly linked to certain cancers. HPV is associated with a range of cancers, including cervical, anal, throat, and penile cancers. By immunizing against HPV, these vaccines effectively reduce the risk of these cancers. The widespread adoption of HPV vaccination has shown a notable decrease in the incidence of cervical cancer, particularly in populations with high vaccination rates. Moreover, ongoing research indicates potential benefits in preventing other HPV-related cancers, further underlining the critical role of these vaccines in cancer prevention strategies.
- Therapeutic Cancer Vaccines: Therapeutic cancer vaccines represent a promising avenue in cancer treatment, targeting specific antigens found on cancer cells. These vaccines are not preventive but are used as a part of treatment for existing cancer. A notable example is the sipuleucel-T vaccine, specifically designed for advanced prostate cancer. This vaccine is customized for each patient, using their own immune cells, which are then exposed to a protein that is part of prostate cancer cells, stimulating the immune system to attack the cancer. The effectiveness of sipuleucel-T in prolonging life expectancy for prostate cancer patients highlights the potential of therapeutic vaccines in managing other types of cancer as well.
- Personalized Neoantigen Vaccines: Neoantigen vaccines take personalization in cancer treatment to the next level. Neoantigens are proteins that arise from cancer cell mutations and are unique to each individual’s tumor, making them ideal targets for the immune system. These vaccines are developed by identifying neoantigens in a patient’s tumor and creating a vaccine to stimulate the patient’s immune system to recognize and attack these specific antigens. This approach ensures that the treatment is highly specific to the patient’s cancer, minimizing the risk of harm to healthy cells. Early clinical trials have shown promising results in various cancers, offering a glimpse into a future where cancer treatment is as unique as the patient’s own genetic makeup.
Immunomodulators: Fine-Tuning the Immune Response
Immunomodulators are substances that adjust the immune system’s activity and come in various forms:
- Checkpoint Inhibitors: These therapies block proteins that serve as checks and balances on immune responses, allowing for a more robust attack on cancer cells. Drugs like nivolumab and pembrolizumab have been successful in treating cancers such as melanoma and non-small cell lung cancer.
- Cytokines: Some cytokines are FDA-approved for various cancers. These proteins, such as interferons and interleukins, modulate the immune system’s response to cancer and have been used in treating kidney cancer and melanoma.
- Agonists: Stimulating the immune system, agonists can enhance the activity of immune cells, providing another avenue for cancer therapy.
- Adjuvants: These substances are used to boost the immune response, potentially improving the efficacy of vaccines.
As research progresses, more immunomodulators are being developed and approved by the FDA, expanding the arsenal of treatments available for cancer patients.
Oncolytic Virus Therapy: A Viral Attack on Cancer
Oncolytic virus therapy marks a unique approach within immunotherapy, utilizing viruses that specifically infect and destroy cancer cells. These viruses are genetically engineered to preferentially target malignant cells, sparing healthy tissue. Additionally, this therapy boosts the immune system’s ability to eradicate remaining cancer cells.
- T-VEC: Leading the Oncolytic Revolution: The FDA’s endorsement of T-VEC, or Imlygic®, is a landmark in oncolytic virus therapy. This therapy uses a modified herpes simplex virus (HSV) tailored to attack melanoma cells. What sets T-VEC apart is its dual action: directly infecting cancer cells and provoking them to produce GM-CSF, an essential protein that stimulates the immune system, thereby enhancing the eradication of cancer cells.
- Mechanism of Oncolytic Viruses: Cancer cells often exhibit weakened antiviral defenses, making them vulnerable to oncolytic viruses. These viruses are tailored to selectively infect and lyse tumor cells, releasing cancer antigens that trigger an immune response against any residual cancer cells.
- Expanding Research and Development: The success of T-VEC in melanoma has opened avenues for exploring various virus platforms in clinical trials. Researchers are assessing different viruses for their potential in treating a range of cancers, each offering unique mechanisms of action suited to specific cancer types. This expanding field promises to bring forward more targeted and effective oncolytic virus therapies.
Targeted Antibodies: Precision Immunotherapy
Targeted antibodies disrupt cancer cell activity and prompt the immune system to eliminate cancer cells. They come in several forms:
- “Naked” Monoclonal Antibodies (mAbs): These antibodies target specific antigens on cancer cells, such as trastuzumab for HER2-positive breast cancer.
- Antibody-Drug Conjugates (ADCs): These carry cytotoxic drugs directly to cancer cells, like ado-trastuzumab emtansine for breast cancer.
- Bispecific Antibodies: These are engineered to engage two different targets simultaneously, such as blinatumomab, which brings T cells into close proximity with cancer cells for acute lymphoblastic leukemia.
These therapies exemplify the precision and potential of personalized medicine in cancer treatment, marking a new era where care is tailored to the individual genetic landscape of each patient’s cancer.
With each advancement, we step closer to a future where immunotherapy doesn’t just treat cancer but does so with unprecedented specificity, reducing side effects and improving quality of life. The journey is complex and full of challenges, but the progress we’ve made fuels our optimism for a brighter, healthier future for all affected by cancer.
Join CRI in Shaping the Future of Immunotherapy
Support the pioneering work of CRI in advancing immunotherapy.