In October of 1962, a young John Ryan walked into a military recruiting station intending to speak with the United States Marine Corps. The Marines seemed like a solid first choice, but the recruiter was on his lunch break. So, Ryan walked next door to the U.S. Navy’s office and signed his name on the dotted line – and began what would become a storied 30-year tenure in the world’s most formidable naval fleet.
I knew where my submarine was… But the free world didn’t.”
Commander John Ryan, USN
The Cloak-and-Dagger Sailor
Ryan had a knack for all things nuclear and in the fall of ‘62, news headlines across the country had three words in common: Cuban Missile Crisis. Ryan knew just where Uncle Sam needed him.
“I did six patrols in the 1960s. I also went to a reactor testing site in Idaho and taught officers and enlisted people how to operate a nuclear submarine in the desert before they went and did it on the open ocean,” Ryan recalled.
After that, the Navy paid for his undergraduate degree and then put him “right back on nuclear submarines. I did six more patrols in the 1970s.”
Much of retired Commander John Ryan’s military service is shrouded in secrecy.
“My campaigns were covert. I knew where my submarine was in the ‘60s and ‘70s and all those thousands of miles we sailed. But the free world didn’t.” The comment rolled off his tongue with a bit of a grin – an understated pride in an impressive career.
Decades spent inside a submarine conjure scenes ripped from the pages of a Tom Clancy novel. When speaking of his service, Ryan is precise and poised, selecting each word with surgical precision. His career of service saw him traverse the oceans of the globe, all while training the next generation of sailors.
In his final years of service before he retired from the Navy in 1992, Ryan was heavily involved in their acquisition contracting officer program. “I started out with very limited experience of negotiating $100 million nuclear overhauls and was involved in various acquisitions of ships and missiles and aircraft,” Ryan said.
His pedigree was impressive, and he soon found himself doing similar work for civilian agencies, that he had done in the military. Ryan eventually retired full time in 2000 to northern Virginia. There, he spent time with his wife, children, and grandchildren and was living the good life.
An Enemy You Can’t See
In April 2013, Ryan’s life took a drastic turn. What began as a routine visit to his primary care physician escalated quickly, landing him in emergency care, where a CT scan revealed a tumor in his left lung. The diagnosis: stage 4 adenocarcinoma, a non-small cell lung cancer (NSCLC) — a life-threatening disease expected to affect almost 200,000 Americans in 2024.
For Ryan, it was an unexpected and frightening moment. He resolved to approach the battle with the same resilience he’d honed over decades of military service.
Initially, chemotherapy was his only option, administered at Walter Reed National Military Medical Center. Yet, as the pain, fatigue, and weight loss persisted with no relief, he questioned if this would be his only option.
Seeking hope, he pursued a second opinion with Dr. William Pao, Chief Oncologist at Vanderbilt-Ingram Cancer Center. Dr. Pao suggested that he consider an innovative approach: immunotherapy.
Ryan found Julie Brahmer, MD, a member of CRI’s Scientific Advisory Council, at Johns Hopkins. There he was enrolled in an immunotherapy clinical trial that would change the course of his life.
The immunotherapy trial began in October 2013 with an initial mix of hope and caution. The first month was rough; residual effects from chemotherapy clung to him—fatigue, pain, and pleural effusion wore him down. But gradually, his body began to respond.
By the nine-week mark, Ryan’s CT scans revealed something astonishing: a 65% reduction in tumor size after just four infusions of nivolumab (Opdivo). The transformative power of immunotherapy was evident, and for the first time, he saw a path forward without the debilitating effects of traditional treatment.
“I thought I’d died and gone to heaven,” Ryan shared, reflecting on the life-changing impact of this treatment.
A Call to Duty
Lung cancer casts a long and deadly shadow over the veteran community. According to the U.S. Department of Veterans Affairs (VA), veterans are at a 25% higher risk of developing lung cancer than the general population—a statistic fueled by their unique exposures to toxic substances during military service. Agent Orange, asbestos, burn pits, and other hazardous materials linger in their bodies long after they’ve left the field.
Combined with historically high smoking rates among service members, these risks create a deadly legacy, with lung cancer remaining the most common cause of cancer-related deaths among veterans. The call to duty has, tragically, also meant a higher likelihood of facing this devastating diagnosis.
Lung cancer in veterans often goes undetected until it reaches its later, more fatal stages. When veterans finally receive a diagnosis, the disease is often so advanced that the chance for survival is heartbreakingly low.
The VA has made strides in earlier detection, implementing low dose computed tomography (LDCT) screenings designed to catch lung cancer early. This program, crucial for veterans with a history of heavy smoking and those over 50, holds promise for saving lives. Early detection could mean the difference between life and death, offering veterans a fighting chance that many haven’t had until now.
Is It Enough?
Veterans have often faced extraordinary health challenges as a result of their service, making access to cutting-edge treatments a critical issue. Gavin Dunn, MD, PhD—a CRI Lloyd J. Old STAR and a Captain in the U.S. Navy Reserves—brings a unique perspective on how military service and a career in medicine and research can intersect to improve patient care for veterans and others affected by cancer.
Dr. Dunn, who leads brain tumor immunology efforts at Massachusetts General Hospital (MGH) in Boston, reflected on how these roles inform each other: “Being a clinician, investigator, and officer all align with my desire to serve others—our patients, our active duty service men and women, and our country,” he said, noting that his journey was inspired by a long family tradition of military service. “It is a privilege to take care of our warriors.”
In addition to his clinical role, Dr. Dunn is committed to advancing cancer immunotherapy and improving treatment access for veterans. “Our veterans represent a group of people who have given much in service to our country,” he explained. “Making sure they have the right access to clinical trial programs is a way that, as a country, we can help repay that service.”
Clinical trials play a critical role in advancing cancer treatments, and Dr. Dunn emphasized their importance for veterans and civilians alike. He advocates for inclusive clinical trial access to all patient communities, with veterans as a particularly important focus.
As Dr. Dunn explained, “Clinical trials are the engine for improving our patients’ lives, helping them live not only longer but with a high quality of life.” This commitment to inclusivity reflects his deep dedication to serving and supporting communities affected by cancer, especially those who have served our country.
(Click here for more information on clinical trials available to veterans and other cancer patients.)
Capping a Legacy of Service in Lands Foreign and Domestic
Back in northern Virginia, Commander John Ryan is settling into his new normal. During the peak COVID years, the pandemic took a toll on him. Yet, his military discipline and resilient spirit saw him through each setback. “The military trained me for resilience, and this was my battlefield,” he said.
When asked what he remembers most about his time receiving immunotherapy treatment, Ryan paused and drew a deep breath. The question seemed to linger through the call like he was measuring his response – that surgical precision he’d spent a lifetime honing. And then the answer became quite clear: time. What cancer survivor doesn’t soak in the time they have?
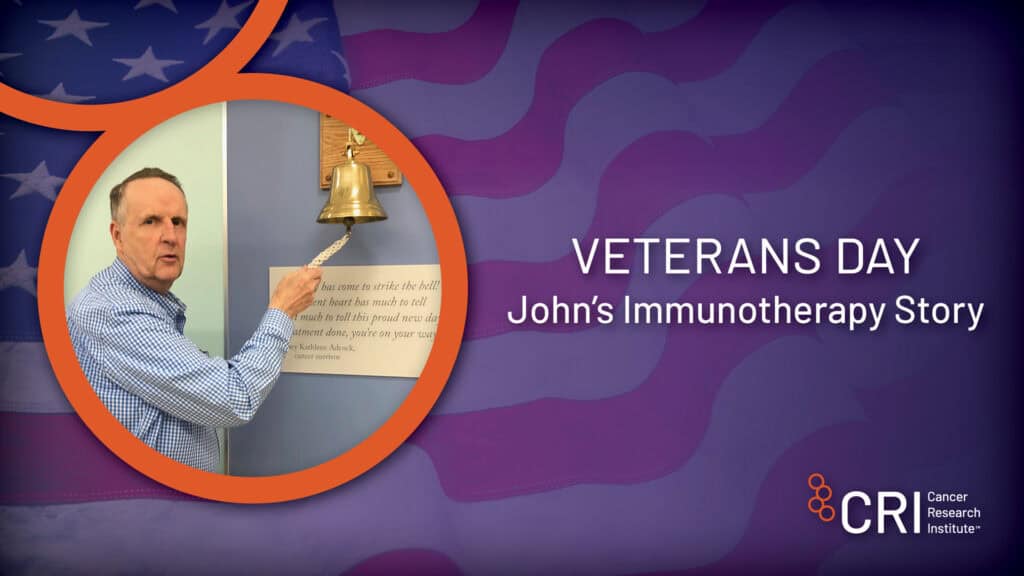
Ryan said his wife has been with him through over 330 trips to Johns Hopkins. He has spent hours and days in chairs receiving infusions– over 225. He’s had close to 70 CT scans. She made the 160-mile round trip with him each time – his foundation.
“When I finally broke out of there and finished those treatments, she went off and joined a ladies’ golf league,” he said with a laugh. “She was crowned the league champion that year.”
These days, he keeps busy with his family. “I have five daughters, three sons, five granddaughters, and three grandsons.” When reflecting on Veterans Day, his voice took a noticeably stoic tone.
“I was rubbing elbows with 16 missile silos, wondering why I was out there,” he said before another signature pause and deep breath. “I was out there for a deterrent force so that we could enjoy freedom.”
