Uniting for a World Immune to Cancer
Together, CRI is turning immunotherapy research into real-world impact by changing the way we treat and defeat cancer.

Power the Research
CRI connects passionate funders and supporters to the science that’s changing cancer care. You are bringing tomorrow’s treatments to patients today.

Sharing Stories of Strength
Meet the patients and caregivers who inspire everything we do. Their journeys show how science, support, and determination are helping more people survive cancer and thrive.
Lead the Next Breakthrough
CRI supports scientists and researchers with the tools to turn bold ideas into real impact. Through funding, trial networks, and shared data, we help accelerate the future of cancer immunotherapy.
Recap of Cancer Immunotherapy Month
Hear survivor stories of hope and resilience, understand the progress in the field of immunotherapy, and learn about the bold research we’re funding at CRI.

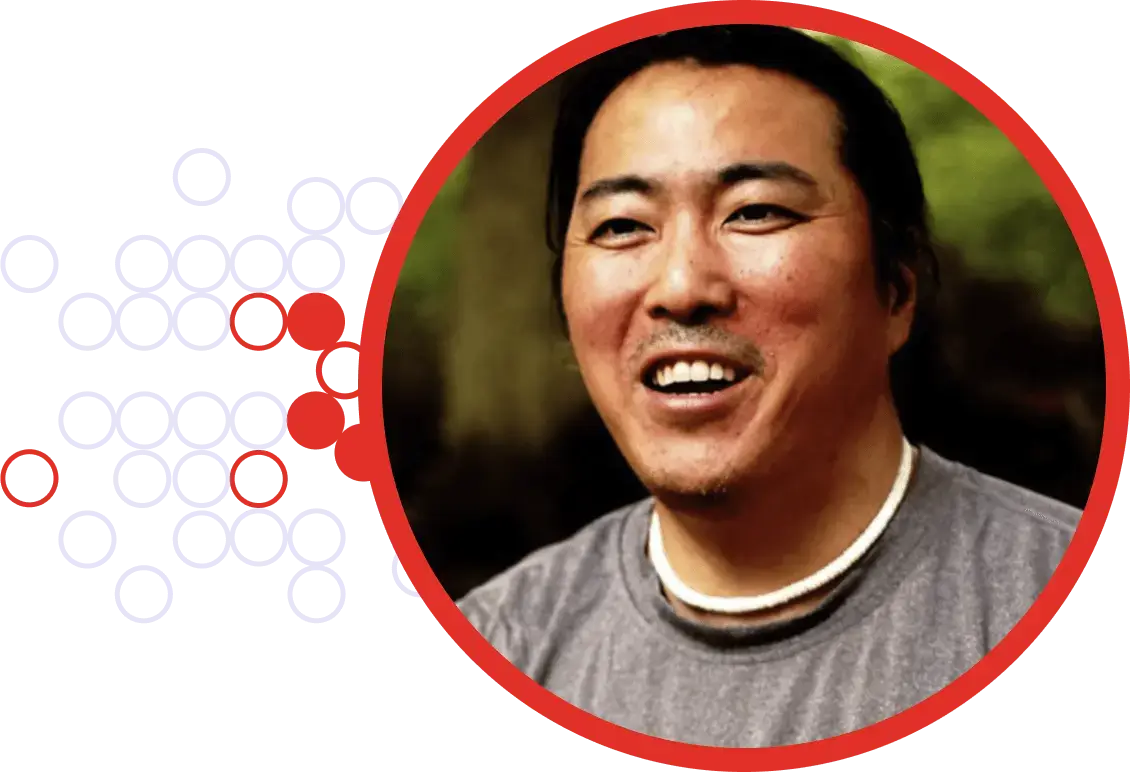
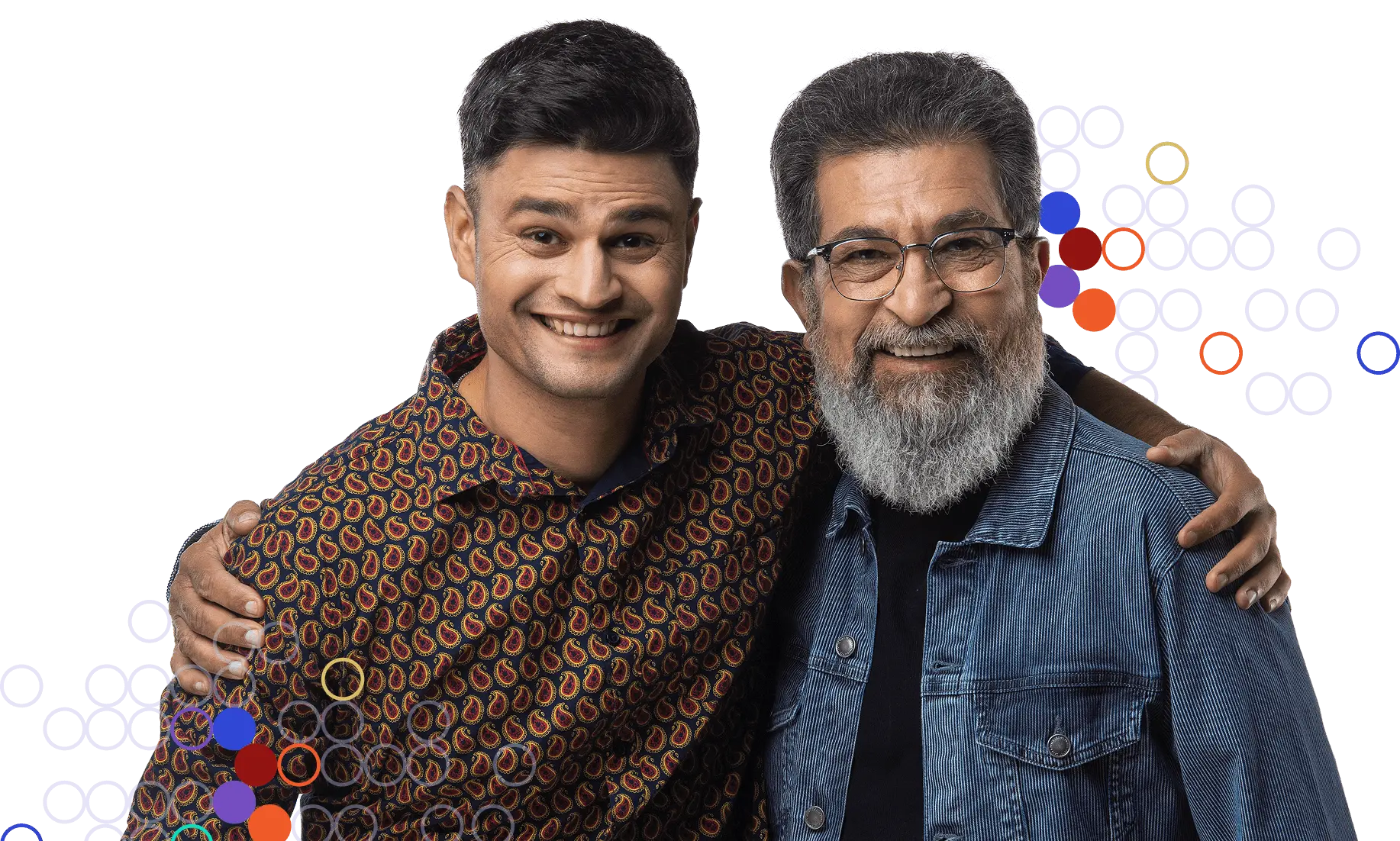
Tom Vibert
Colorectal Cancer Survivor
Accelerating Science That Saves Lives
Tom’s tumor shrank more from a single dose of immunotherapy than from two years of chemotherapy.
Our Impact
Turning Research Into Results
Immunotherapy Stories
In these inspiring stories, patients, scientists and supporters share their personal experiences with cancer. Their stories offer wisdom and hope to all those affected by cancer.

“I’m hoping I’m really doing my part to one day find a cure or find a way to prevent cancer from impacting the lives of so many people.”
Keith Doubman
Funder & Supporter
Our partners
Conquering
Cancer Together
We cultivate lasting strategic partnerships with research institutions, cancer treatment centers, biopharmaceutical companies, and nonprofits to facilitate innovation in IO and advance new lifesaving immunotherapies for more patients.
News and Events
Discover how we are building a world without cancer on our news and events page.
Join CRI in Shaping the Future of Immunotherapy
Support the pioneering work of CRI in advancing immunotherapy.