The first batch of NY-ESO-1 recombinant protein produced in a facility supported entirely by non-profit entities has successfully cleared regulatory review and has entered clinical testing. The clinical trials are part of the Cancer Vaccine Collaborative, a joint program of the Cancer Research Institute, Inc. (CRI) and the Ludwig Institute for Cancer Research Ltd. (LICR).
Patients with ovarian cancer in one study and with melanoma in a second study are receiving the cancer vaccine containing the protein. Both clinical trials are being performed to assess the safety and the anti-tumor immune response of the NY-ESO-1-specific therapeutic cancer vaccine alone and in combination with other agents. Drs. Nina Bhardwaj and Anna Pavlick are the principal investigators of the melanoma trial at the New York University Medical Center. Dr. Kunle Odunsi is the principal investigator of the ovarian cancer vaccine trial at the Roswell Park Cancer Institute in Buffalo, NY.
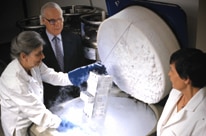
The NY-ESO-1 protein was produced at the LICR / Cornell University Partnership Production Facility in Ithaca, New York, in which LICR has invested over $9 million. The partnership, which was initiated in 2001 by Dr. Lloyd J. Old, director of the Cancer Vaccine Collaborative, when he was scientific director of the LICR, is one of the few non-commercial Good Manufacturing Practice (GMP) production facilities in the USA that is capable of producing recombinant proteins for clinical use.
Dr. Old points out that scientists are confronted with a frustrating set of barriers when their discoveries need to be tested for therapeutic benefit in humans. “The paramount challenge is obtaining the potential drug or vaccine in a form that can be used in man and that has passed the myriad safeguards set up to protect humans from injury,” says Dr. Old. “Almost without exception, the entire process is under the control of companies, where commercial priorities by necessity predominate.”
“The manufacturing of clinic-ready NY-ESO-1 by the Cornell production facility, and the initiation of clinical trials with this vaccine component, show that academic institutions can take control of this essential step in translating laboratory discovery into clinical realities,” says Dr. Old. “Exploring this model more broadly would greatly enhance the participation of the academic community in drug development and bring the remarkable advances of fundamental research more rapidly to the benefit of patients.”
Professor Carl Batt, director of the LICR / Cornell University Partnership Production Facility, and his team have established the core competencies required for production of recombinant proteins using microbial expression systems P. pastoris (yeast) and E. coli (bacteria). Professional staff and graduate students work side-by-side at the facility in production campaigns that last many weeks (see «About GMP Production» below).
In 1997, Dr. Old and LICR Affiliate Yao-Tseng Chen at the Weill Cornell Medical College in New York, discovered the NY-ESO-1 cancer/testis antigen, which was shown in LICR studies to be expressed by many different cancer types. NY-ESO-1 has been the central focus of CRI/LICR Cancer Vaccine Collaborative investigations, and its immunogenicity has been studied in more than 40 early phase, single variable clinical trials.
In June of 2009, the Cancer Research Institute awarded a two-year grant of $450,000 to Cornell University to support the cGMP production of clinic grade MELAN-A protein. MELAN-A, also called MART-1, is an antigen found on melanocytes—a type of skin cell that produces melanin, the pigment that colors human flesh—and on melanoma tumors derived from these skin cells. It is known that the immune system can recognize MELAN-A, which has been the topic of many laboratory and clinical studies. The protein is slated to be used in planned CRI/LICR Cancer Vaccine Collaborative clinical trials of vaccines for melanoma.
About GMP Production
While individual “campaigns” (productions) are quite different, the components of the process are largely the same:
- First, “process development” is conducted in the Ithaca facility’s Bioprocess Development Laboratory. This is the step in which the performance of the expression system is optimized and scale-up to production level is tested. Every effort is made to duplicate standard Biological Production Facility (BPF) operating conditions, from equipment to reagents to temperatures.
- Once process development has been completed, the expression system and processes are transferred to the BPF section of the facility for GMP-compliant production of small amounts of clinic-grade recombinant proteins.
GMPs, or current GMP (cGMP), are the international standards and controls that govern manufacturing and quality control testing for pharmaceuticals, biologics, medical devices and foods. GMPs are enforced by national regulatory agencies, including the Food and Drug Administration (FDA) in the USA, the Therapeutic Goods Administration (TGA) in Australia, and the Agência Nacional de Vigilância Sanitária (National Health Surveillance Agency; ANVISA) in Brazil.
GMP, Good Laboratory Practice (GLP) and Good Clinical Practice (GCP) together form “GxP’ requirements. GxPs form the basis of the standard operating procedures and activities of the Institute’s Office of Clinical Trials Management, which handles administrative oversight for most CRI/LICR Cancer Vaccine Collaborative clinical trials.
News Coverage of this Release
Cornell University working on vaccine to fight cancer — WSYR-TV Syracuse, Sept. 1, 2009
Cancer vaccine ready for testing — News 10 Now TV Syracuse, Aug. 14, 2009
Related Articles
CU-Ludwig facility opens for producing anti-cancer agents November 13 — Cornell University Chronicle, Nov. 7, 2002
CU-Ludwig partnership produces a new cancer-drug facility within Stocking Hall — Cornell University Chronicle, Nov. 21, 2002
Researchers Try to Cut New Path to Pharmacy — Wall Street Journal, Jan. 12, 2004
Media Contact
Brian Brewer, Director of Communications
Cancer Research Institute
(212) 688-7515 ext. 242 or [email protected]
About the CRI/LICR Cancer Vaccine Collaborative
The Cancer Vaccine Collaborative is a partnership between two not-for-profit institutions, the Cancer Research Institute (CRI) and the Ludwig Institute for Cancer Research (LICR). Each of these institutions has a long and distinguished history in the field of cancer immunology and each is committed to translating laboratory discoveries in this field into therapeutic cancer vaccines. Begun in 2001, the CRI/LICR Cancer Vaccine Collaborative supports and coordinates a network of early phase cancer vaccine trials at nineteen hospitals and medical centers around the world. Driven by a scientific agenda, these parallel, single-variable trials use defined antigens, standard treatment protocols, uniform monitoring methodologies, and centralized data collection to provide comparable results that are teaching us how to effectively immunize against cancer.
About the Ludwig Institute for Cancer Research
The Ludwig Institute for Cancer Research (LICR) is an international non-profit institute dedicated to understanding and controlling cancer. With operations at 73 sites in 17 countries, the LICR network quite literally spans the world. LICR has developed an impressive portfolio of reagents, knowledge, expertise, and intellectual property, and has also assembled the personnel, facilities, and practices necessary to patent, clinically evaluate, license, and thus translate, the most promising aspects of its own laboratory research into cancer therapies. Visit https://www.licr.org for more information.